
In a systematic review 47% of patients in mental health services had experienced physical abuse and 37% had experienced sexual abuse. In the household survey in England and Wales, adults who had experienced four ACEs were twice as likely to attend their general practice repeatedly, compared with those with no ACEs history, and incidence of health service use rose as the ACEs experiences increased. Individuals and families who have experienced violence and trauma seek support from healthcare and other services for the physical, psychological and socioeconomic consequences of trauma. In a systematic review and meta-analysis of 37 observational studies of health behaviours and adult disease, patients with four or more ACEs were at higher risk of a range of poorer health outcomes including cardiovascular disease and mental ill health, versus those with no ACEs history. The links between cumulative adversity from ACEs, DVA and other traumatic experiences are explained within the ecobiodevelopmental framework and the concept of toxic stress. Ĭumulative trauma across the lifespan is associated with multiple health consequences.
Up to 29% women and 13% men have experienced DVA in their lifetime, at a cost of £14 billion a year to the UK economy. DVA is considered to be a chronic and cumulative cause of complex trauma. In England, a household survey found that nearly half of adults had experienced at least one ACE, including childhood sexual, physical or verbal abuse, as well as household domestic violence and abuse (DVA). Adverse childhood experiences (ACEs) are stressful or traumatic events that occur during childhood or adolescence. People experiencing socio-economic disadvantage, women, minoritized ethnic groups, and the LGBTQ + community are disproportionally affected by violence and trauma. The WHO World Mental Health Survey identified that 70% of participants had experienced lifetime traumas, including physical violence, intimate partner sexual violence, and trauma related to war. Individual, interpersonal and collective trauma is a highly prevalent and costly public health problem.
GUIDING PRINCIPLE OF INTERVENTION TRAUMA DIRECTED CARE PROFESSIONAL
ConclusionsĪ coordinated, more centralized strategy and provision for TI healthcare, increased funding for evaluation, and education through professional networks about evidence-based TI health systems can contribute towards evidence-informed policies and implementation of TI approaches in the UK. Professionals had conflicting views on the future of TI approaches, however all agreed that government backing is essential for implementing policies into practice. We identified factors affecting implementation of TI approaches at the level of organization (leadership, service user involvement, organizational culture, resource allocation, competing priorities) and wider context (government support, funding). Professionals wanted enhanced coordination between organizations and regions. TI care in the UK has had piecemeal implementation, with a nation-wide strategy and leadership visible in Scotland and Wales and more disjointed implementation in England. Although documents and interviews provided differing interpretations of TI care, they were aligned in describing the integration of TI principles at the system level, contextual tailoring to each organization, and addressing varied challenges within health systems. TI approach was included in national, regional and local policies, however, there was no UK- or NHS-wide strategy or legislation, nor funding commitment.

We analysed 24 documents and interviewed 11 professionals from healthcare organizations and local authorities. We used the Ready Extract Analyse Distil (READ) approach to guide policy document review, and the framework method to analyse data.

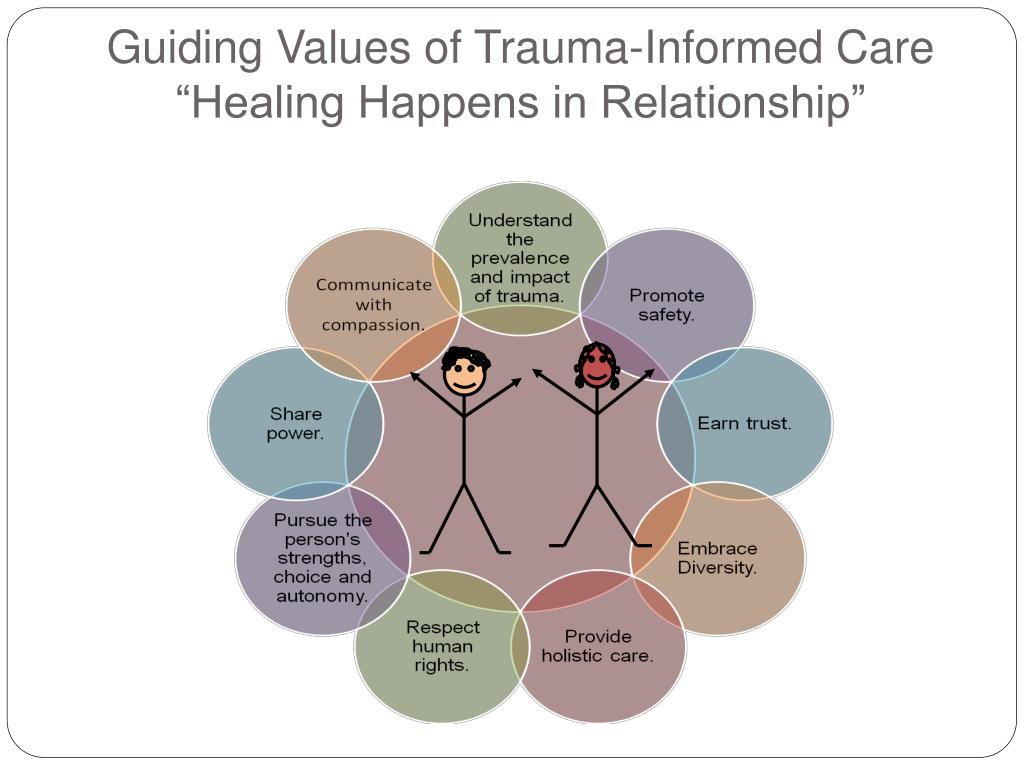
MethodsĪ qualitative study comprising of a document analysis of UK health policies followed by semi-structured interviews with key informants with direct experience of developing and implementing TI approaches. This study aimed to investigate the UK-specific context through exploring how TI approaches are represented in health policies, and how they are understood and implemented by policy makers and healthcare professionals. Review of TI approaches in primary and community mental healthcare identified limited evidence for its effectiveness in the UK, however it is endorsed in various policies. Trauma-informed (TI) approach is a framework for a system change intervention that transforms the organizational culture and practices to address the high prevalence and impact of trauma on patients and healthcare professionals, and prevents re-traumatization in healthcare services.


 0 kommentar(er)
0 kommentar(er)
